Hearing the word “cancer” can turn your world upside down. However, here’s something important—technology in cancer care has undergone significant changes in recent years. Radiation therapy, once feared for its side effects, has evolved into a precise, AI-driven, and patient-friendly treatment option.
For breast and lung cancer patients, this progress has been life-changing. With advanced tools and smarter systems, treatment today can target tumours more accurately, protect healthy tissues, and reduce side effects.
And if you’re in Kolkata, an experienced radiation oncologist like Dr. Mukti Mukherjee brings these innovations right to your care plan.
Why Radiation Oncology Needed a Tech Revolution
Traditional radiation therapy definitely works—but advancement in technology makes it more accurate. The traditional method can sometimes expose healthy organs to radiation, leading to fatigue, skin reactions, or damage to nearby tissues. Modern radiation oncology advancements in 2025 are changing that picture.
Machines today are faster, smarter, and guided by real-time imaging and Artificial Intelligence. For both breast cancer radiation therapy innovations and lung cancer radiation treatment, this means treatment that’s safer and far more precise.
The Breakthroughs Powering Modern Cancer Care
Below is a compact table summarising major recent technologies and how they help specifically in breast and lung cancer:
| Innovation | What It Does | Benefits of Breast / Lung Cancer |
| IGRT (Image-Guided Radiation Therapy) | Uses imaging (CT, X-ray, cone beam) just before or during treatment to confirm tumour position | Adjusts for breathing motion (especially in lungs), ensures that the dose hits the tumour and spares healthy tissues |
| SBRT (Stereotactic Body Radiotherapy) | Delivers very high doses in fewer, precise sessions | Useful for small lung nodules or oligometastasis; less treatment burden |
| Proton Therapy for Cancer | Uses protons (charged particles) rather than X-rays | Can spare adjacent organs (heart, ribs, lung), especially in left breast or in central lung lesions |
| AI in Radiation Oncology | Uses machine learning to plan, adapt, and predict outcomes | Speeds up contouring (drawing tumour/organ outlines), adapts radiation plan mid-course, and predicts side effects |
| Adaptive Radiation Therapy | Adjusts the plan over the treatment course based on changes (tumour shrinkage, weight change) | Keeps treatment accurate even as the body/tumour changes |
| Radiation Side Effect Management Tools | Tools (imaging biomarkers, predictive AI models) to foresee and reduce side effects | Reduces risks of pneumonitis, fibrosis, and skin damage |
1. Image-Guided Radiation Therapy (IGRT)
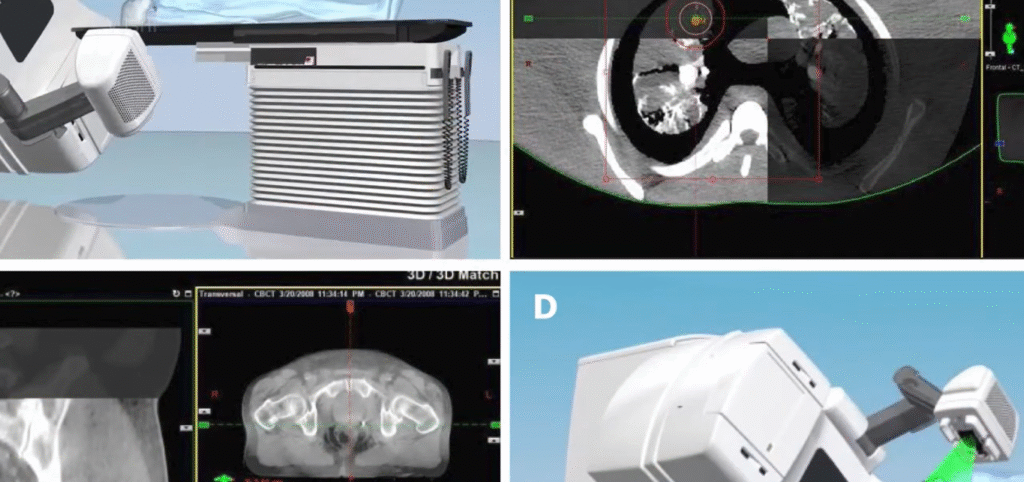
One of the most significant innovations is Image-Guided Radiation Therapy (IGRT). This technology captures images right before or during treatment, ensuring radiation is hitting exactly where it should.
This is especially vital in lung cancer radiation treatment, where tumours move as you breathe. IGRT helps track that motion and adjust the beam in real time. It’s like having a GPS that never lets the radiation drift off-course.
2. Stereotactic Body Radiotherapy (SBRT)
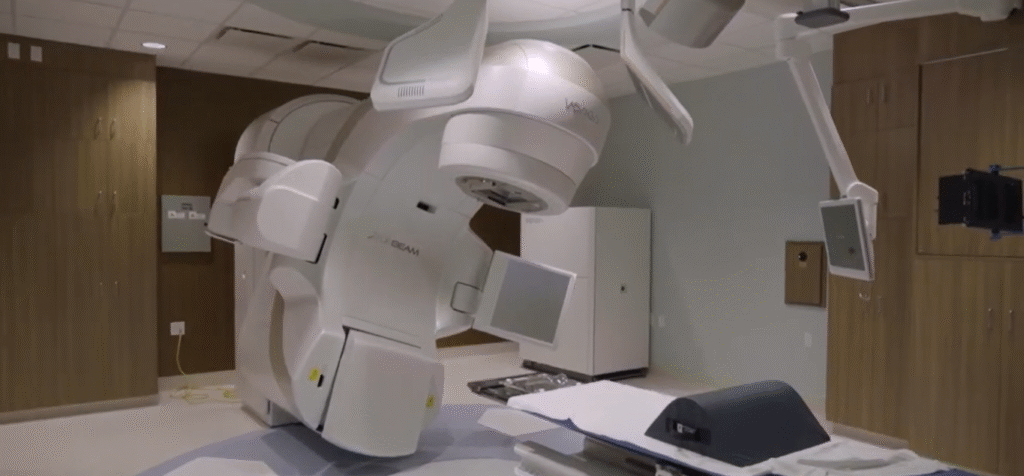
Stereotactic Body Radiotherapy (SBRT) delivers high doses of radiation in just a few precise sessions. This is a big relief for patients who would otherwise need weeks of daily treatment.
For small lung tumours or limited metastases, SBRT offers accuracy so fine that it’s almost surgical—but without a single incision. It’s transforming outcomes while reducing patient fatigue and treatment time.
Proton Therapy: Power and Precision
One of the most talked-about frontiers is proton therapy for cancer. Unlike traditional X-rays, proton beams release most of their energy directly inside the tumour and then stop. That means nearby organs—like the heart, lungs, or healthy breast tissue—receive minimal radiation.
This precision is especially valuable for left-sided breast cancer, where the heart lies close to the chest wall. Though still available at select centres, proton therapy is a symbol of how far radiation oncology has come in reducing long-term risks.
4. Artificial Intelligence in Radiation Oncology
AI in radiation oncology is more than a buzzword—it’s transforming how doctors plan and deliver treatment.
AI can now:
- Map tumours and organs automatically, saving time and improving accuracy.
- Predict side effects before they occur, allowing preventive action.
- Adapt treatment plans mid-therapy if the tumour shrinks or the anatomy changes.
This level of automation and learning makes radiation therapy faster, safer, and deeply personalised.
5. Personalised Cancer Treatment
No two cancers are the same. Personalised cancer treatment tailors therapy based on your tumour type, genetics, and body anatomy.
For breast and lung cancer patients, this approach means radiation doses, techniques, and even treatment schedules are customised for your unique condition. With adaptive planning and AI, doctors like Dr. Mukti Mukherjee, an expert radiation oncologist in Kolkata, can adjust your plan in real time as your tumour responds.
How Technology Reduces Side Effects
One of the biggest worries about radiation therapy has always been side effects. Thankfully, radiation side effect management has evolved just as fast as the treatment itself.
- Smarter planning tools now limit how much radiation nearby organs receive.
- Imaging biomarkers detect early signs of tissue irritation, allowing for quick intervention.
- AI-based prediction models identify who’s at risk of fatigue or inflammation before symptoms start.
The result? Less damage, faster recovery, and a better quality of life during and after treatment.
The Role of Technology in Breast Cancer Radiation
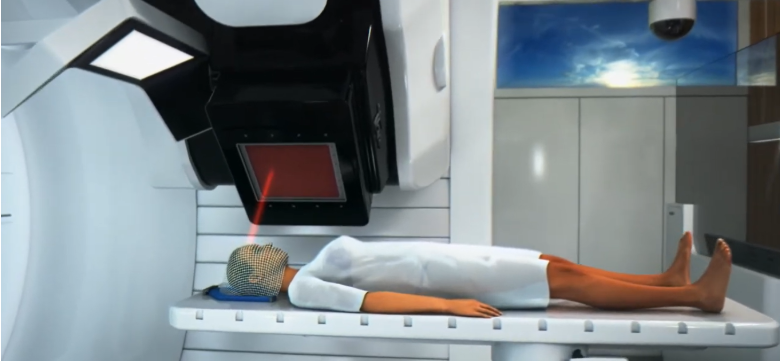
Breast cancer radiation therapy has seen a complete transformation. Techniques like deep inspiration breath-hold (where patients hold their breath for short periods) move the heart away from the chest wall during treatment, drastically reducing exposure.
Add IGRT and proton therapy to that mix, and treatment becomes not just effective but safer. These breast cancer radiation therapy innovations allow doctors to deliver the right dose exactly where it’s needed while keeping healthy tissue almost untouched.
The Role of Technology in Lung Cancer Radiation
Lung tumours are tricky—they move when you breathe and sit close to delicate tissues. Advanced lung cancer radiation treatment uses motion tracking, gating, and SBRT to overcome this challenge.
- Motion management systems synchronise treatment with your breathing cycle.
- IGRT verifies tumour position before each dose.
- Adaptive planning adjusts treatment as the tumour responds.
Together, they make radiation not only effective but also safer than ever before.
The Future of Cancer Care Technology
The future of cancer care technology looks even more exciting. Researchers are working on:
- Real-time tumour tracking using MRI-guided radiation systems (MR-Linac).
- FLASH therapy, which delivers an ultra-high radiation dose in milliseconds, potentially minimises damage to normal tissue.
- Genomic-guided radiotherapy, using genetic information to customise radiation doses.
- AI-driven predictive analytics, helping doctors fine-tune every millimetre of a radiation plan.
These upcoming radiation oncology advancements in 2025 will make treatments shorter, safer, and even more effective.
Why a Skilled Specialist Matters
Technology alone doesn’t save lives—it’s the expertise behind it that makes all the difference. A skilled radiation oncologist in Kolkata, like Dr. Mukti Mukherjee, ensures that these advanced tools are used correctly and compassionately.
With years of experience treating breast and lung cancer, Dr. Mukherjee integrates AI in radiation oncology, IGRT, SBRT, and proton therapy for cancer into her practice to give patients precise, comfortable, and customised care.
What Patients Should Ask Their Doctor
If you or a loved one is facing breast or lung cancer, don’t hesitate to ask these important questions:
- Does the doctor use IGRT, SBRT, or adaptive radiation therapy?
- How are side effects monitored and managed?
- Can the treatment plan change mid-therapy if needed?
Understanding these aspects can help you make confident, informed choices.
People Also Ask
What is Image-Guided Radiation Therapy (IGRT)?
IGRT uses imaging during treatment to guide radiation beams precisely to the tumour. It accounts for body movements like breathing and helps protect healthy tissues.
How does SBRT help in lung cancer?
SBRT delivers very high doses of radiation in a few sessions, targeting the tumour with extreme precision. It’s especially effective for small lung tumours or early-stage cancers.
Is proton therapy better than traditional radiation?
Proton therapy is more precise. It stops right at the tumour, causing minimal exposure to nearby organs. It’s especially useful for cancers near sensitive structures like the heart or brain.
Can AI really help in radiation therapy?
Yes. AI helps doctors plan treatments faster, predict side effects, and adapt therapy as your body changes—making the process more efficient and personalised.
What is the future of radiation oncology?
The future includes real-time imaging, MRI-guided systems, FLASH therapy, and genetics-based planning. These innovations promise shorter treatments with fewer side effects and better results.