“Why would my doctor recommend radiation therapy for liver cancer? I thought only surgery or chemotherapy worked.”
If that sounds familiar, you’re not alone. Liver cancer is often misunderstood, and so is radiation therapy. Many patients assume surgery or chemotherapy are the only options. But modern radiation therapy has become a safe, precise, and life-improving treatment. This is especially for those who cannot undergo surgery.
As a radiation oncologist in Kolkata, Dr. Mukti Mukherjee combines medical expertise with compassion, guiding patients through every step. Read this post to understand how radiation therapy works for liver cancer.
What is Radiation Therapy for Liver Cancer?
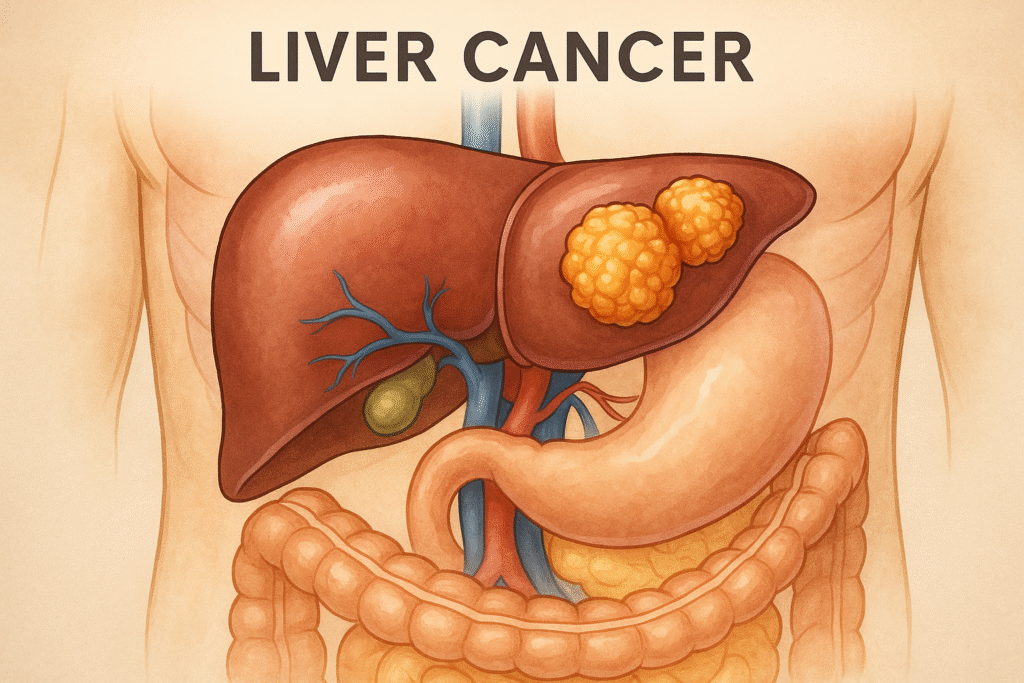
Radiation therapy uses high-energy beams, such as X-rays or protons. These target and destroy cancer cells in the liver. Unlike chemotherapy, which circulates throughout the body, radiation is localised. It focuses directly on the tumour while sparing nearby healthy tissues.
Radiation therapy is often recommended when:
- Surgery isn’t possible due to tumour size, location, or patient health.
- Tumours are near vital organs or major blood vessels.
- Cancer has returned after previous treatments.
- The goal is symptom relief, tumour shrinkage, or growth control.
This is how radiation shrinks tumours, minimises pain, and improves quality of life. This makes it a valuable option even when surgery isn’t suitable. Many patients who once thought they had limited options now see real improvements.
Types of Radiation Therapy for Liver Cancer
Different liver tumours need different approaches. Here’s a closer look at the most commonly used therapies:
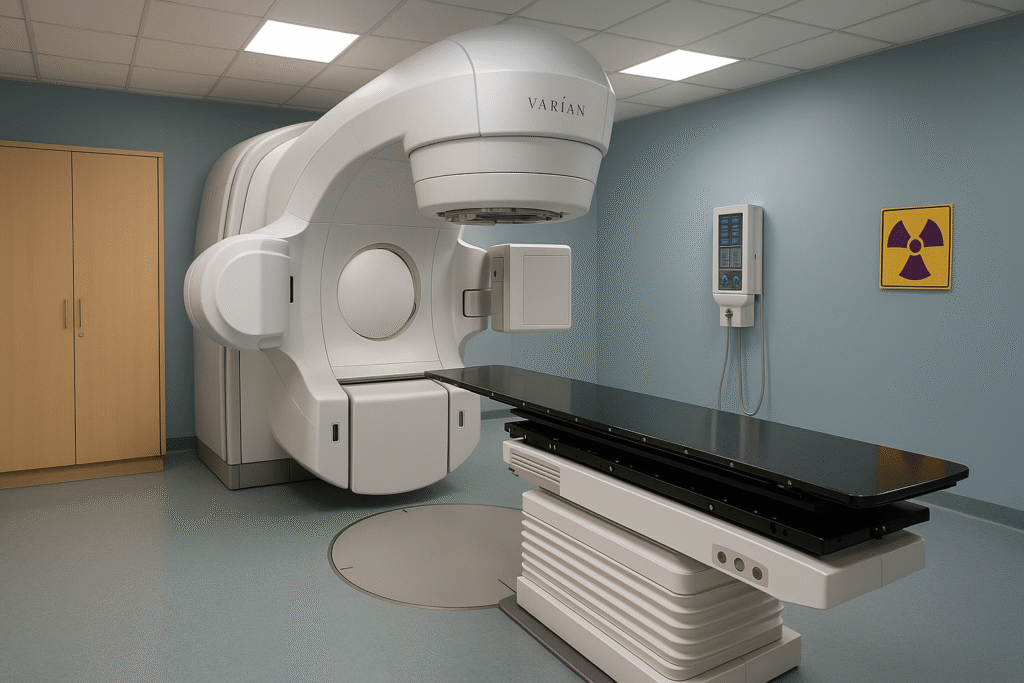
1. External Beam Radiation Therapy (EBRT)
- Delivered from outside the body using specialised machines.
- Non-invasive and typically administered over several sessions.
- Focuses precisely on the tumour, minimising damage to healthy liver tissue.
It is the starting point for those who need controlled, safe treatment over several weeks. It’s suitable for both small and moderate liver tumours. Patients appreciate that EBRT allows daily life to continue with minimal interruption.
2. Stereotactic Body Radiation Therapy (SBRT)
- Ideal for small, inoperable tumours.
- Shorter overall treatment time compared to traditional radiation.
- Extremely precise, reducing the risk to healthy liver tissue.
- Often combined with other treatments like chemotherapy or ablation.
SBRT has emerged as a game-changer for liver cancer patients with a high control rate. Many patients report less fatigue and quicker recovery.
3. 3D Conformal Radiation Therapy (3DCRT)
- Uses 3D imaging to map the tumour’s exact shape.
- Radiation beams are shaped to the tumour’s contours.
- Protects the surrounding healthy liver tissue from unnecessary exposure.
3DCRT is helpful for larger tumours or those located near sensitive structures. It offers a layer of safety. Patients often find comfort knowing the therapy is done based on their unique anatomy. This reduces the risks of complications.
How Modern Radiation Therapy Achieves Accuracy
Today, liver cancer radiation therapy relies on image-guided technology and real-time monitoring. This allows a radiation oncologist in Kolkata to:
- Track liver movement during breathing.
- Adjust beams daily to account for subtle shifts.
- Plan the dose carefully to ensure safety for healthy liver tissue.
These advancements make radiation a reliable treatment even for patients with complex cases. With technology guiding each step, patients feel more secure about their care.
The Liver Cancer Radiation Therapy Process
Understanding the process step-by-step can make treatment less intimidating:
Step 1: Consultation
- Review of scans, blood tests, and health.
- Assessment of tumour size, liver function, and prior treatments.
- Creation of a personalised radiation plan.
- Patients can ask questions and understand why radiation is preferable over other therapies.
Step 2: Simulation
- A CT scan maps the tumour and surrounding tissues.
- Marks or custom moulds ensure precise alignment.
- This step ensures radiation hits the exact target every session.
Step 3: Treatment Sessions
- Usually delivered for few days a week over several weeks.
- Each session takes about 15–30 minutes.
- Sessions are pain-free, though some patients notice mild fatigue.
- Many patients can continue daily routines with minor adjustments.
Step 4: Monitoring and Follow-up
- Blood tests and imaging track treatment response.
- Side effects like mild nausea or skin redness are managed promptly.
- Adjustments to the plan ensure maximum safety.
- Continuous monitoring ensures both tumour control and liver health.
Benefits of Radiation Therapy for Liver Cancer
Radiation offers a lot of advantages, particularly for patients ineligible for surgery:
- Shrinks tumours before surgery or transplant.
- Relieves symptoms such as pain or bile duct obstruction.
- Non-invasive and outpatient-friendly.
- Minimal disruption to daily routines.
- It can be done with chemotherapy or ablation for greater efficacy.
Radiation therapy can be a lifesaving option, providing control over tumour growth. It also helps preserve liver function. Patients often describe feeling more in control of their treatment journey.
When Surgery Isn’t an Option
Surgery is not a good option for some liver cancers due to:
- Tumour location near critical structures
- Underlying liver disease, such as cirrhosis
- Other medical conditions that increase surgical risk
In these cases, SBRT or 3DCRT can:
- Control tumour growth.
- Reduce pressure on internal organs.
- Provide a safe alternative to surgery.
Radiation is also effective when cancer recurs after surgery or ablation. It offers hope for continued management. Patients who were told they had no options can benefit from radiation therapy.
Managing Side Effects
While modern radiation is safe, some side effects may occur:
Short-term:
- Fatigue
- Mild nausea
- Skin redness
- Appetite loss
Long-term (rare):
- Liver function changes
- Radiation-induced liver disease
Tips for recovery:
- Stay hydrated and eat light, nutritious meals
- Avoid alcohol
- Rest when needed
- Keep in regular contact with the radiation oncologist in Kolkata
Dr. Mukti Mukherjee ensures that each patient receives support both medically and emotionally. This can make a significant difference in recovery.
Emotional Support Matters Too
Liver cancer can be overwhelming. Many patients report feeling anxious, fearful, or uncertain.
Dr. Mukti Mukherjee emphasises clear communication and patient empowerment. It helps patients feel informed and confident. Patients often describe the care as “compassionate, reassuring, and thorough.”
Emotional safety plays a key role in treatment adherence and outcome. Understanding the why and how behind each treatment step helps patients cope better.
Who is Suitable for Radiation Therapy?
Patients may be suitable if they:
- Have early-stage, inoperable liver cancer.
- Need symptom control in advanced stages.
- Have recurrent tumours after prior treatment.
- Prefer fewer side effects than surgery or chemotherapy.
Radiation is particularly helpful for:
- Single tumors
- Cases awaiting liver transplant
- Combination treatment plans
Long-Term Recovery and Results
- Follow-up imaging in 6–8 weeks
- Regular blood tests monitor liver function and tumour markers
- Maintenance treatment may be needed
Expected outcomes:
- Tumour shrinkage
- Symptom relief
- Improved quality of life
- Long-term tumour control in select cases
Patients report more energy, less pain, and confidence in their treatment plan.
Why Choose Dr. Mukti Mukherjee?
- Expert radiation oncologist in Kolkata
- Specialised in liver cancer treatment
- Uses SBRT, 3DCRT, and IGRT for precise therapy
- Offers complete medical and emotional support
- Highly rated for compassionate, clear communication
Dr. Mukti believes no patient should feel rushed, judged, or afraid. Every step is explained and monitored.
Book Your Consultation Today
Consult Dr. Mukti Mukherjee, a radiation oncologist in Kolkata, for a personalised liver cancer treatment plan.
People Also Ask
- Is radiation therapy painful?
No, treatment is painless. Some fatigue may occur.
- Can it cure liver cancer?
In early-stage cases or with combination therapies, yes. Otherwise, it controls tumour growth.
- How long does it take?
Most plans last 6-8 weeks; SBRT may finish in 3–5 sessions.
- Can radiation be repeated?
Yes, with careful planning and liver monitoring.
- Does it affect liver transplant eligibility?
No, it can help control tumours while awaiting a transplant.
- What is the success rate?
SBRT offers up to 90% local control in early or small tumours.